My BEST Dentists Journal

Dentists and dental students are among providers now authorized to administer COVID-19 vaccine nationwide
The U.S. Department of Health and Human Services is amending an emergency declaration under the Public Readiness and Emergency Preparedness Act to authorize additional providers, including dentists and dental students, to vaccinate patients for COVID-19 nationwide, according to a March 11 announcement in the Federal Register.
To date, at least 26 states already enlist dentists to administer the COVID-19 vaccines during the COVID-19 public health emergency. The federal declaration allows licensed dentists throughout the country to vaccinate the public against COVID-19, regardless of state laws that prevent dentists from doing so.
The Association sent a Feb. 11 letter to HHS on this issue and the ADA was also part of a September 2020 coalition letter asking for the same liability protection.“Dentists already have the requisite knowledge and skills to administer vaccines and observe side effects — and many do so on a daily basis,” wrote ADA President Daniel J. Klemmedson, D.D.S., M.D., and ADA Executive Director Kathleen T O’Loughlin, D.M.D., in the February letter. “Dentists are well educated in human anatomy, physiology, and pathophysiology, and are trained to administer intra-oral local anesthesia.
It is arguably more difficult to administer an inferior alveolar nerve block inside the oral cavity than to vaccinate an exposed arm and manage any side effects.”The White House said March 11 the administration will be expanding the pool of qualified professionals able to administer shots to include dentists and other providers. And during his presidential address that night, President Joe Biden announced a goal to make “every adult in the U.S. eligible for vaccination no later than May 1.”

He also vowed to increase the number of places Americans can get vaccinated, including increasing the total number of participating community health centers to 950, and plans to double the number of federally-run mass vaccination centers.The Public Readiness and Emergency Preparedness Act, or PREP Act, allows the Health and Human Services Secretary to issue a declaration in a public health emergency.
This declaration provides temporary immunity from tort liability claims (except willful misconduct) to individuals or organizations involved in the manufacture, distribution or dispensing of medical countermeasures, which may include vaccines. This declaration may be amended as circumstances warrant. During the COVID-19 public health emergency, a declaration was first issued in January 2020 by former HHS Secretary Alex Azar.
On March 11, Acting HHS Secretary Norris Cochran amended the declaration to designate additional health care professionals, including dentists and students, as "qualified persons” whom are authorized to administer COVID-19 vaccines.
Other qualified providers include midwives, paramedics, EMTs, physician assistants, respiratory therapists, podiatrists, optometrists and veterinarians. The amended declaration also includes retired or nonpracticing health care providers who have had active licenses or certifications within the last five years as long as they were in good standing prior to the license becoming inactive, expired or lapsed.
For information about COVID-19 vaccinations, the ADA has created a fact sheet for dentists and dental team members about the status and safety of COVID-19 vaccines. The ADA continues to monitor developments related to COVID-19 vaccine authorization and administration on behalf of the profession and public. Visit ADA.org/virus for the latest information.
(03/12/2021)by ADA
More Information: https://www.mybestdentists.com/resources/AmericanDentalAssociation
Views: 3,051
DDS and DMD: What Is The Difference?
DDS and DMD are the acronyms of the degrees dentists earn after finishing dental school. DDS means Doctor of Dental Surgery, and DMD can mean either Doctor of Medicine in Dentistry or Doctor of Dental Medicine. While the names are different, the American Dental Association (ADA) explains that they represent the same education. Some universities may grant dental graduates with a DDS, and others grant a DMD, but both degrees have the same requirements.
According to the ADA, the Baltimore College of Dental Surgery established the first Doctor of Dental Surgery degrees in 1840. When Harvard University started its dental school in 1867, their degrees were called Dentariae Medicinae Doctorate (Doctor of Medicine in Dentistry) because Harvard uses Latin names for their degrees. Even though these degrees are based on the same educational requirements, they still have different names.
What Is the Difference Between a DDS and a DMD?

Today, many universities award a DMD degree. Dentists with either a DDS or a DMD are educated to practice general dentistry. All dentists receive a rigorous education. First, dental schools typically require a four-year undergraduate education. Afterward, graduates go to dental school for another four years of classroom training, clinical training, and dental laboratory training.
Dental students spend the first two years of dental school studying biomedical sciences courses like anatomy, biochemistry, pathology, and pharmacology. The last two years are focused on clinical and laboratory training.

After graduating from dental school, dentists must pass a national written examination called the National Board Dental Examination, followed by a regional clinical board examination. Dentists must also pass a jurisprudence examination about state laws before being given a license to practice dentistry in that state.
With such extensive education and examination requirements, you can be certain that any dentist with a DDS or DMD degree is qualified to treat you.
Education After a DDS or DMD
Most dentists stick with practicing general dentistry. However, some choose to specialize in a particular area of dentistry after earning their degree. Training programs range from two to six years, depending upon the specialty area. There are several dental specialties, including endodontics, orthodontics, periodontics, prosthodontics, oral surgery, and pediatric dentistry. The ADA can help you find a dentist with a specialty that fits you best.
Dentists receive a rigorous education and have to pass several exams to be able to practice. Whether they have a DDS or DMD after their name, you should choose a dentist based on their skills, types of services provided, communication, and professionalism.
(03/03/2021)by ADA
More Information: https://www.mybestdentists.com/resources/AmericanDentalAssociation
Views: 2,957
Family Dental Practice: What It Is And The Best Way To Find One
Everyone in your family has unique oral care needs throughout their lives. The good news is that there are dental offices that cater to various family oral care needs! You just have to know where to look and what to ask for. Learn more about family dental groups and why they may be a good fit for you.
Family dentist vs. General dentist
Family dentistry has been around for a long time. But family dental offices are unique because they provide a variety of treatments in-house. According to the American Dental Association (ADA), most dentists in North America – about 158,000 – practice general dentistry. General dentists can treat most oral care issues for the whole family, and they are considered your primary care dentist. Many general dentists have specialties, like orthodontics, root canal therapy, or even cosmetic dentistry.
Family dental groups or practices typically offer specialties or services for the whole family at the same location. With family dentists, you can schedule appointments for multiple family members at the same time. Of course, this depends on the schedule and availability of the dental office. Still, you can ask offices when searching for a family dentist. Having this kind of scheduling ability means less time waiting for back-to-back appointments or appointments on multiple days.

Benefits of a family dentist
Family dental groups are popular because they are so versatile. Most family dental groups have multiple dentists in their practice, offering the convenience of a "one-stop" solution for all your family's oral care needs. Suppose you need a pediatric dentist, an endodontist, or an orthodontist. In that case, you can find family dentists that provide all three in one office.
Family dental groups can make dentist visits positive experiences for children, especially. Children should have a dentist and dental hygienist who are gentle, patient, and comfortable working with kids. Kind and gentle dentists and dental hygienists will keep children comfortable and encouraged. It's worth the effort to find the perfect dental professional that makes your kids feel comfortable so they can have a lifelong positive attitude toward dental appointments.
How to find a state-of-the-art family dental practice
Many family dental groups have efficient and modern technology and facilities. All you have to do is research what you need and ask offices what they offer. Ask about the procedures and equipment the office uses when choosing your family dentist.
Today, many dental groups prefer safer X-ray machines and better imagining software to show patients any issues. This technology is called intraoral camera exams. The dentist can magnify problem areas on a monitor using a small camera. These are just two examples of modern technology found at most dental offices.
Intraoral cameras and newer X-ray machines are less invasive, which can really help children with dental anxiety. Check with your insurance carrier and research treatment plans when choosing a family dentist to ensure there are no surprises.
How to find a family dentist
A good family dental group will have worked with adults and kids, including very young children. You should search for a family dentist who can understand and respond to your family's various needs, such as losing those first teeth, fluoride needs, and even tooth whitening for the adults.
Consider the following as you are looking for a family dental group:
List the needs of your family members. Will one child need braces while another needs only a regular cleaning? Some dental groups have both a general dentist and orthodontist in the office.
Does the group have a pediatric dentist on-site? Pediatric dentists treat young children, young patients with special needs or disabilities.
Experience and rapport are vital for a long-term relationship. Read the family dental practice's website to read biographies, specialties, and services offered. You can ask friends and family for recommendations and read reviews online.
You should be able to ask questions and bring up concerns to your dentist and dental hygienist, including asking for product recommendations, healthy snack ideas, and demonstrations of flossing skills. You should learn more about preventative oral care and teach your children proper oral care habits with help from the family dental group.
Aside from experience and rapport, there are some convenience factors to look for as well:
Is the family dental group located close to home?
Are you able to schedule appointments conveniently, and do they send reminders?
What are the payment options available, including financing for procedures not covered by dental insurance?
Is the dental team professional and caring with their patients?
You can search for dentists in your area through reputable sites like the American Dental Association (ADA) Mouth Healthy site. Don't be afraid to be picky about your dentist. A family dental group can provide dental care to your whole family throughout your children's lives.
(02/26/2021)by ADA
More Information: https://www.mybestdentists.com/resources/AmericanDentalAssociation
Views: 3,086
As part of its ongoing COVID-19 vaccine strategy, the ADA supports recognizing dentists as vaccine providers
The ADA and state dental societies are advocating giving dentists the ability to be an integral part of stopping the spread of the COVID-19 pandemic, with at least 20 states allowing dentists to administer the vaccine.
“As part of its ongoing COVID-19 vaccine strategy, the ADA supports recognizing dentists as vaccine providers,” said ADA President Daniel J. Klemmedson, D.D.S., M.D. “Having dentists administer vaccines in their communities helps improve the public vaccination rate, and it relieves some of the burden on the current vaccine provider network.”
The ADA House of Delegates passed Resolution 91H-2020 in October, which acknowledged that dentists have the requisite knowledge and skills to administer critical vaccines that prevent life- or health-threatening conditions.

“Because most of the states have recognized dentistry as essential, it is only fitting that we join front-line workers in the ability to administer the vaccine,” said David M. White, D.D.S., ADA Council on Government Affairs chair.
“We are just very proud to be recognized as essential.”States and territories are continuing to refine their COVID-19 vaccination plans following the Food and Drug Administration’s Dec. 11, 2020, authorization of the first COVID-19 vaccine, with efforts possibly including the use of dentists to assist with vaccination efforts. Final authority rests with each state in prioritizing the population to receive the vaccine and in administering it.
Working with state dental societies, the ADA has developed an interactive map that details dentists’ ability to administer the COVID-19 vaccination by state, as well as the phase of the state vaccination plan in which dentists will receive the COVID-19 vaccination.Dr. White said advocacy occurred at two levels. “We have advocated on the federal level through ADA Government Affairs to ask the Department of Health and Human Services to allow dentists to administer the COVID-19 vaccine,” he said.

“More recently advocacy has occurred on the state level to change laws for dentists to administer all vaccines.” To help states in introducing legislation to allow dentists to administer vaccines, the ADA has developed principles to aid state associations in advocating for this expansion of the scope of practice.
“The state Government Affairs department at the ADA provides assistance to the states on model legislation and strategy for successfully passing laws,” Dr. White said.The ADA vaccine principles include participating in an online vaccination administration course, establishing patient relationships, complying with record-keeping requirements and falling under immunity statutes within the state.
They are available at ADA.org/principles.Karin Irani, D.D.S., California Dental Association trustee, volunteered on a day off to administer vaccines at a Los Angeles “Mega POD,” large-scale points of vaccination distribution chosen for their regional accessibility and ability to process thousands of people daily.
“This is the time for dentists to rise to the challenge and show our medical colleagues and the legislatures how dentists can contribute to the community's health,” Dr. Irani said. “State dental societies and the ADA should continue their advocacy efforts so dentists are recognized as an essential health care provider. The general population and the local authorities are starting to recognize dentists' importance in providing overall health care.”
(02/04/2021)by ADA
More Information: https://www.mybestdentists.com/resources/AmericanDentalAssociation
Views: 3,076
Can Acid reflux be related to the erosion of my teeth?
Did you know your digestive health can affect your teeth?
Frequent stomach upset can cause a gradual wearing away of the protective enamel on your teeth, a process known as tooth erosion. This can affect the appearance of your teeth and open the door for harmful bacteria that cause cavities.
How Do Stomach Problems Affect My Teeth?

Your stomach produces natural acids that help your body digest food. Sometimes, these acids travel up the throat and into the mouth, especially after a large meal. Ordinarily, our saliva rebalances the acid levels in our mouth and everything’s fine.

But for those who suffer from gastroesophageal reflux, also known as acid reflux or GERD, gastric acids reach the mouth throughout the day. This process is especially damaging when you’re asleep, since you are swallowing less often and your mouth is producing less saliva.
Another concern is the dry mouth caused by many acid reflux medicines. Saliva not only helps neutralize the acids caused by acid reflux, but also helps to wash away food particles and reduce bacteria that attack tooth enamel. This is why lower saliva production may increase your risk for cavities.
What Does Reflux-Related Erosion Do to My Teeth?
Acid reflux can wear away the enamel on the inside surfaces of your teeth, as well as the chewing surfaces. Your dentist may notice this during an exam.
Unfortunately, tooth erosion is permanent. If your enamel has started to wear away, you may:
Feel pain or sensitivity when consuming hot, cold or sweet drinks
Notice a yellowish discoloration of the teeth
Find that your fillings have changed
Face greater risks for cavities over time
Develop an abscess, in extreme cases
Experience tooth loss, also in extreme cases
Once erosion occurs, you may need fillings, crowns, a root canal or even tooth removal. Veneers may be an option to restore the look of your smile.
How to Protect Your Teeth – And Get Relief
Chewing sugar-free gum can encourage saliva production, which helps neutralize and wash away the acids in your mouth. Look for one with the ADA Seal of Acceptance.
Prescription or over-the-counter fluoride and desensitizing toothpastes may help strengthen tooth enamel.
Avoiding alcohol and smoking and refraining from eating 3 hours before bedtime may reduce the frequency of acid reflux episodes.
If heartburn, acid reflux or other stomach problems are part of your daily life, work with your physician on a care plan to treat the underlying causes of your stomach troubles.
If you suffer from acid reflux, see your dentist regularly so they can make sure your teeth stay healthy, recommend ways to prevent tooth enamel erosion and suggest ways to get relief if you are also suffering from dry mouth.
(01/26/2021)by ADA
More Information: https://www.mybestdentists.com/resources/AmericanDentalAssociation
Views: 3,130
When and how often should you brush your teeth?
The American Dental Association recommends brushing your teeth twice a day with fluoride toothpaste for two minutes each time.
When you brush your teeth, you help remove food and plaque — a sticky white film that forms on your teeth and contains bacteria. After you eat a meal or snack that contains sugar, the bacteria in plaque produce acids that attack tooth enamel.
Eventually, the acid can break down tooth enamel, causing cavities. Plaque that isn't removed can also harden into tartar, making it harder to keep teeth clean. Tartar buildup on your gums leads to inflammation that causes gum disease.

In choosing when to brush your teeth, you might also consider your diet. If you've eaten an acidic food or drink, avoid brushing your teeth right away. These acids weaken tooth enamel, and brushing too soon can remove enamel.
If you have arthritis or have difficulty holding a toothbrush, consider buying an electric or battery-operated toothbrush. These have been shown to remove plaque better than manual toothbrushes.
Besides brushing your teeth, to keep your mouth healthy, do the following:
Floss daily.
Use mouthwash after brushing and flossing.
Drink plenty of water.
Eat a healthy diet and limit sugary food and drinks.
Avoid frequent snacking.
Replace your toothbrush every three to four months, or sooner if the bristles are irregular or splayed.
Schedule regular dental checkups with X-rays and cleanings.
(12/14/2020)by ADA
More Information: https://www.mybestdentists.com/resources/AmericanDentalAssociation
Views: 3,117
Cancer and Dental Health
More than one-third of all cancer patients develop complications that affect the mouth, according to the National Institute of Dental and Craniofacial Research. These mild to severe side effects can include mouth sores, infection, dry mouth, sensitive gums and jaw pain.
Your mouth health is an important part of your overall health, so make your dentist part of your cancer care team. If you don’t have a regular dentist, use the ADA Find-A-Dentist tool to search for an ADA member dentist in your area.

How Cancer Affects Your Mouth:
Cancer and its treatments, like chemotherapy, can weaken your immune system. If your mouth is not as healthy as possible prior to your cancer treatment, you may be more susceptible to infection. If the infection is serious enough, it can delay your cancer treatment. In addition, radiation therapy, especially in the area of the head and neck, can damage salivary glands which can cause thick, sticky saliva and extreme dry mouth. A dry mouth can increase your chances of tooth decay and infection.
Maintaining your mouth at its best health before, during and after cancer treatment could help lessen some side effects and allow you to focus on your overall healing.
If your mouth is not as healthy as possible prior to your cancer treatment, you may be more susceptible to infection. If the infection is serious enough, it can delay treatment.
Your dentist can evaluate your dental health and discuss which treatment options you should consider prior to starting cancer treatment. By treating areas of concern you may reduce possible dental side effects associated with chemotherapy and radiation. Some treatment options may include fluoride treatments to prevent cavities, filling existing cavities, treating gum disease, removing infected teeth or restoring crowns or bridge work to ensure you will be able to chew your food.
During the course of your cancer treatment you may experience mild to severe side effects. Be sure to consult with your cancer care team prior to dental checkups, especially if you have a port under your skin for receiving medication or feeding. This is important because patients with a port may also take anti-blood clotting medications, which can increase bleeding during dental and medical procedures and the risk of infection.
After cancer treatment, you may find yourself experiencing some dental issues or simply needing a regular checkup. As you're working toward your best health, don't forget to take care of your mouth. After all, it is the gateway to the rest of your body.
Visit Your Dentist:
Routine check-ups and cleanings are essential, so visit your dentist on a regular basis. Due to the effects of cancer treatment, you may have moderate to severe tooth decay as a result of dry mouth since saliva (spit) is essential in rinsing the mouth of food particles and plaque. Treatment may include filling cavities, root canals, or crown and bridge work.
(12/09/2020)by ADA
More Information: https://www.mybestdentists.com/resources/AmericanDentalAssociation
Views: 3,274
It’s important to realize that your dentist sees much more than just your teeth
Many Americans today enjoy excellent oral health and are keeping their natural teeth throughout their lives. But this is not the case for everyone. Cavities are still the most prevalent chronic disease of childhood.
Too many people mistakenly believe that they need to see a dentist only if they are in pain or think something is wrong, but they're missing the bigger picture. A dental visit means being examined by a doctor of oral health capable of diagnosing and treating conditions that can range from routine to extremely complex.

A Team Approach
The team approach to dentistry promotes continuity of care that is comprehensive, convenient, cost effective and efficient. Members of the team include dental assistants, lab technicians and dental hygienists. Leading the team is the dentist, a doctor specializing in oral health who has earned either a Doctor of Dental Medicine (DMD) degree or a Doctor of Dental Surgery (DDS) degree, which are essentially the same.

The Dentist's Role
Dentists are doctors who specialize in oral health. Their responsibilities include:
Diagnosing oral diseases, Promoting oral health and disease prevention, Creating treatment plans to maintain or restore the oral health of their patients, Interpreting x-rays and diagnostic tests, Ensuring the safe administration of anesthetics, Monitoring growth and development of the teeth and jaws, Performing surgical procedures on the teeth, bone and soft tissues of the oral cavity.
More than Just Teeth and Gums
Dentists' areas of care include not only their patients' teeth and gums but also the muscles of the head, neck and jaw, the tongue, salivary glands, the nervous system of the head and neck and other areas. During a comprehensive exam, dentists examine the teeth and gums, but they also look for lumps, swellings, discolorations, ulcerations — any abnormality. When appropriate, they perform procedures such as biopsies, diagnostic tests for chronic or infectious diseases, salivary gland function, and screening tests for oral cancer.
In addition, dentists can spot early warning signs in the mouth that may indicate disease elsewhere in the body. Dentists' training also enables them to recognize situations that warrant referring patients for care by dental specialists or physicians.
Education and Clinical Training
The level of education and clinical training required to earn a dental degree, and the high academic standards of dental schools, are on par with those of medical schools and are essential to preparing dentists for the safe and effective practice of modern oral health care.
Most dental students have earned Bachelor of Science degrees or their equivalent, and all have passed rigorous admission examinations.
The curricula during the first two years of dental and medical schools are essentially the same — students must complete such biomedical science courses as anatomy, biochemistry, physiology, microbiology, immunology and pathology. During the second two years, dental students' coursework focuses on clinical practice — diagnosing and treating oral diseases.
Why Oral Health Matters
Numerous recent scientific studies indicate associations between oral health and a variety of general health conditions — including diabetes and heart disease. In response, the World Health Organization has integrated oral health into its chronic disease prevention efforts "as the risks to health are linked."
The American Dental Association recommends that dental visits begin no later than a child's first birthday to establish a "dental home." Dentists can provide guidance to children and parents, deliver preventive oral health services, and diagnose and treat dental disease in its earliest stages.
Dentists' areas of care include not only their patients' teeth and gums but also the muscles of the head, neck and jaw, the tongue, salivary glands, the nervous system of the head and neck and other areas.
(12/08/2020)by ADA
More Information: https://www.mybestdentists.com/resources/AmericanDentalAssociation
Views: 3,174
HIV/AIDS and Dental Health
If you, or someone you know, is living with HIV/AIDS, the American Dental Association recommends that dental health care be part of all HIV/AIDS treatment plans. That’s because people living with HIV/AIDS are more susceptible to infections including dental infections, which can affect their overall health.
What Is HIV/AIDS?

HIV (human immunodeficiency virus) is a virus that attacks a specific type of T cell known as CD4 cells. T cells are an important part of the body’s immune system which is needed to fight infection. If left untreated, HIV can destroy so many CD4 cells that a person can no longer fight off infections and disease. AIDS (acquired immunodeficiency syndrome) is the last state of HIV infection where the immune system is so very weak that infection and cancer can take over.
How Does HIV/AIDS Affect the Mouth?

Your mouth may be the first part of your body to be affected when infected with HIV. Because infection with HIV will weakened your immune system, this means you will be susceptible to infections and other problems. In your mouth, this can cause pain and tooth loss. People with HIV may experience the following mouth issues:
Dry mouth
Thrush
White lesions on the sides of the tongue (oral hairy leukoplakia)
Red band gingivitis
Ulcerative periodontitis
Karposi’s Sarcoma
Outbreaks of herpes simplex virus
Canker sores
Mouth ulcers
Dental and mouth problems related to HIV can be painful, which can cause trouble chewing or swallowing. This may prevent you from taking your HIV medication. It can also result in malnutrition, as you may have trouble eating and absorbing enough essential nutrients. A compromised digestive system may affect the absorption of your HIV drug treatment.
How Can I Cope with Dental and Mouth Issues Related To HIV?
Most mouth health problems related to HIV are treatable. Talk to your dentist about what treatment is best for you. The best ways to prevent these issues are to do the following:
Visit your dentist for regularly scheduled appointments.
Brush and floss your teeth twice daily for two minutes.
Take your HIV medicine on schedule.
Tell your doctor if your HIV medicine is causing dry mouth. Ask what treatment is best for you.
If you do not have a regular dentist, ask your primary care provider or clinic for a referral.
(11/14/2020)by ADA
More Information: https://www.mybestdentists.com/resources/AmericanDentalAssociation
Views: 3,283
Diabetes and Your Smile
Did you know that 29.1 million people living in the United States have diabetes? That’s 9.3% of the population. Approximately 1.7 million new cases are diagnosed each year—and 8.1 million people living with diabetes don’t even know they have it.Diabetes affects your body’s ability to process sugar. All food you eat is turned to sugar and used for energy. In Type I diabetes, the body doesn’t make enough insulin, a hormone that carries sugar from your blood to the cells that need it for energy. In Type II diabetes, the body stops responding to insulin. Both cases result in high blood sugar levels, which can cause problems with your eyes, nerves, kidneys, heart and other parts of your body.So what does this have to do with that smile of yours — and how can you protect it? First, it’s important to understand the signs of diabetes and the roles they play in your mouth.
The Symptoms of Untreated Diabetes
The warning signs of diabetes affect every part of your body. After a blood test, you may be told by a doctor that you have high blood sugar. You may feel excessively thirsty or have to urinate a lot. Weight loss and fatigue are other common symptoms. Diabetes can also cause you to lose consciousness if your blood sugar falls too low.If diabetes is left untreated, it can take a toll on your mouth as well. Here's how:

You may have less saliva, causing your mouth to feel dry. (Dry mouth is also caused by certain medications.)
Because saliva protects your teeth, you’re also at a higher risk of cavities.

Gums may become inflamed and bleed often (gingivitis).
You may have problems tasting food.
You may experience delayed wound healing.
You may be susceptible to infections inside of your mouth.
For children with diabetes, teeth may erupt at an age earlier than is typical.
Why People with Diabetes Are More Prone to Gum Disease
All people have more tiny bacteria living in their mouth now than there are people on this planet. If they make their home in your gums, you can end up with periodontal disease. This chronic, inflammatory disease can destroy your gums, all the tissues holding your teeth and even your bones.Periodontal disease is the most common dental disease affecting those living with diabetes, affecting nearly 22% of those diagnosed. Especially with increasing age, poor blood sugar control increases the risk for gum problems. In fact, people with diabetes are at a higher risk for gum problems because of poor blood sugar control. As with all infections, serious gum disease may cause blood sugar to rise. This makes diabetes harder to control because you are more susceptible to infections and are less able to fight the bacteria invading the gums.
How Your Dentist Can Help You Fight Diabetes
Regular dental visits are important. Research suggests that treating gum disease can help improve blood sugar control in patients living with diabetes, decreasing the progression of the disease. Practicing good oral hygiene and having professional deep cleanings done by your dentist can help to lower your HbA1c. (This is a lab test that shows your average level of blood sugar over the previous three months. It indicates how well you are controlling your diabetes.)
Your Diabetes Dental Health Action Plan
Teamwork involving self-care and professional care from your dentist will be beneficial in keeping your healthy smile as well as potentially slowing progression of diabetes. Here are five oral health-related things you can do to for optimal wellness:
Control your blood sugar levels. Use your diabetes-related medications as directed, changing to a healthier diet and even exercising more can help. Good blood sugar control will also help your body fight any bacterial or fungal infections in your mouth and help relieve dry mouth caused by diabetes.
Avoid smoking.
If you wear any type of denture, clean it each day.
Make sure to brush twice a day with a soft brush and clean between your teeth daily.
See your dentist for regular checkups.
(10/21/2020)
by ADA
More Information: https://www.mybestdentists.com/resources/AmericanDentalAssociation
Views: 3,148
What to eat when you're having dental issues
You know that what you eat directly impacts your health, and that includes the health of your teeth and gums. But it can work the other way around too. If you have an orthodontic appliance, such as braces, or have had certain dental problems or procedures, the health and comfort of your teeth and gums can directly impact what you eat. Here are some tips for what to eat and how to avoid these common dental issues.
Braces are delicate, and any food that you need to bite into to eat is prime for breaking braces. You can get around this by cutting the food, such as corn off the cob or rib meat off the bone, or slicing apples and chopping carrots into small, bite-size pieces.

Any food that you need to bite into to eat is prime for breaking braces. You can get around this by cutting the food, such as corn off the cob or rib meat off the bone, or slicing apples and chopping carrots into small, bite-size pieces. You may also experience problems eating after your braces are tightened–teeth may feel sore.
The first few days are the worst, so try eating softer foods like those listed below until the soreness passes: Scrambled eggs,oatmeal, soup with soft vegetables or pureed or cream soups, soft cheeses, including cottage cheese, smoothies and milkshakes, pudding and custard, meatloaf, mashed potatoes, sorbet and frozen yogurt, tortillas (soften by microwaving or steaming), yogurt, soft-cooked, shredded chicken and meat, protein shakes, tofu, ripe fruits, such as peaches and nectarines, cut into bite-size pieces, couscous, quinoa, bulgur, soft-cooked rice, pasta and noodles, polenta, baked apples, peanut butter, chicken or tuna salad, refried beans, avocado , applesauce, macaroni and cheese, pancakes, soft bread, saltines and matzoh, mashed bananas, cooked veggies, hummus, canned or cooked fruit.

If you get mouth sores, try these tips to make eating easier and speed healing: Choose cool or room temperature foods, blend and moisten dry or solid foods, drink through a straw to bypass mouth sores, eat high protein, high calorie foods to speed up healing time. For example, add protein powder to milk shakes or powdered dry milk to fortify mashed potatoes and soups.
Your nutrition and dietary needs following oral surgery or getting implants depends on factors including your nutritional status prior to your procedure, the extent of your procedure, how much impact there is on oral function and how long your recovery is expected to last. A liquid or soft foods diet may be required for a few days or longer, until your mouth heals. Opt for nutrient-rich foods such as fruits, vegetables, low-fat dairy foods and lean meats, eggs and beans whenever possible since they provide vitamins, minerals and nutrients needed for healing, including zinc, protein, and vitamins A and C.
Try these foods: Scrambled eggs, oatmeal or cream of wheat (make with milk instead of water to boost nutrition), soup with soft vegetables or pureed or cream soups, soft cheeses, including cottage cheese, smoothies and milkshakes, pudding and custard, meatloaf, mashed potatoes (fortify by mixing in powdered milk to boost nutrition, sorbet and frozen yogurt, tortillas (soften by microwaving or steaming), yogurt, soft-cooked, shredded chicken and meat, protein shakes, tofu,ripe fruits, cut into pieces like peaches and nectarines, peanut butter, saltines and matzoh, mashed bananas, cooked veggies, like carrots, squash, green beans, spinach and other greens, spinach soufflé, hummus, canned or cooked fruit.
Swallowing problems can occasionally happen, but if it persists, talk to your doctor since it could be related to something serious. Causes of swallowing issues vary and treatment depends on what is causing the problem. If you are having trouble swallowing, to prevent choking and aspiration avoid these foods: Alcoholic beverages, extremely hot foods and beverages, caffeine, spicy foods, popcorn, bran cereal, nuts, cottage cheese (unless pureed), skins of fruits, celery, dry, crumbly, or sticky foods (such as bread, cake, peanut butter, banana).
Depending on level of swallowing difficulty, the following foods may be included in the diet. These foods are grouped into four different categories:
Thin liquids that dissolve quickly in the mouth such as frozen yogurt, ice cream, gelatin and broth.
Nectar-like liquids where liquid coats and drips off a spoon such as nectars, milkshakes, cream soup and vegetable juices.
Honey-like liquids that flow off a spoon in a ribbon like in yogurt, tomato sauce and honey.
Spoon-thick liquids that are thickened to pudding consistency such as pudding, custard or hot cereal.
(09/30/2020)by ADA
More Information: https://www.mybestdentists.com/resources/AmericanDentalAssociation
Views: 3,288
ADA Practice Transitions expands nationally in October
When Dr. Shanna L. Gagnon was looking for an associate dentist to join her practice, she considered one factor as the most important in finding a successful hire: practice philosophy.
“Personality definitely plays a role as well, but if the doctor and the new associate do not have the same philosophy of care, it will not work out,” she said. To ensure she found an associate with a similar practice philosophy in her search, Dr. Gagnon decided to try a new service offered by the ADA a try.“I took the ADAPT application very seriously and put a lot of thought into it as I filled out my profile,” she said. “I figured that the more complete and honest the profile, the more likely I would be matched with the right candidate.”

In July, Dr. Gagnon officially welcomed Dr. Jessica Sikora to her practice, Gagnon Dental in Farmingdale, Maine. The two were matched by ADA Practice Transitions (ADAPT), a service backed by the ADA focused on helping dentists make the process of joining or leaving a practice predictable and successful. This occurred as Dr. Sikora neared graduation from the University of New England College of Dental Medicine earlier this year.
Come October, dentists nationwide will be able to take advantage of the ADA Practice Transitions like Drs. Gagnon and Sikora.The service announced Sept. 9 it is expanding its services to all 50 states and is encouraging dentists to answer three quick questions at ADAPracticeTransitions.com to become an ADAPT Insider and receive early access to create a profile before the October opening. By filling out the form, dentists will also be entered to win a $100 Amazon gift card.

Dr. Gagnon, who serves on the Maine Dental Association board of directors, was impressed by a presentation on ADA Practice Transitions last fall, and began her profile right away, as Maine was an early pilot state for ADA Practice Transitions.
“I could not be happier with my new associate, Dr. Sikora,” she said. “It is very obvious that the ADA has done their homework in attempting to set up a successful matching service.”ADA Practice Transitions piloted the service in Wisconsin, Maine, Indiana, Iowa, Kentucky, Michigan, Minnesota and New Hampshire for dentists seeking to join or purchase a practice in those states who are looking to hire an associate or find someone to purchase their practice.
“ADA members, volunteer leaders and state associations all over the country have expressed interest in what ADA Practice Transitions is doing, and so we are happy to be able to expand nationally,” said Dr. Kirk Norbo, ADA Business Innovation Group board chair. “Part of the value of ADA Practice Transitions is its ability to use the platform to match dentists nationwide for those who are seeking to move to a different state. We anticipate that over time, the ADA Practice Transitions platform and methodology will become the first choice for dentists seeking a transition.”
Through ADA Practice Transitions, dentists receive:
• Matches with dentists or practices that aligns with their personal and professional goals.
• Step-by-step support from a dedicated ADA advisor.
• Customized resources and help defining the right path.
ADA Practice Transitions helps retiring owners find the right person to continue to care for their patients, and helps owners hire associates who share a similar philosophy of care, ensuring a successful transition and continuity of care for patients.In addition, ADA Practice Transitions helps buyers and associates find the practice that fits their criteria and shares their goals.
ADA Practice Transitions can also help a dentist explore and narrow down their options to provide more confidence in taking their next steps.
(09/12/2020)by ADA
More Information: https://www.mybestdentists.com/resources/AmericanDentalAssociation
Views: 3,162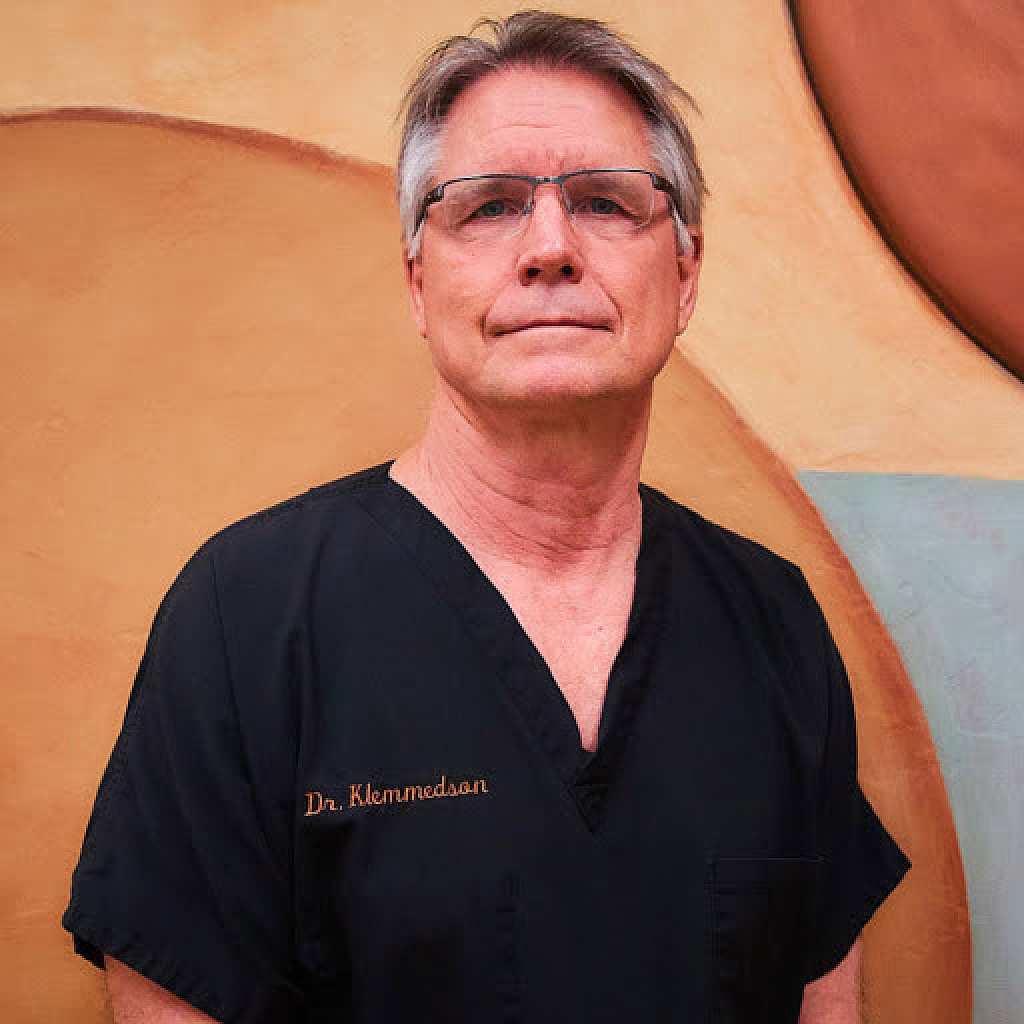
Dr. Daniel J. Klemmedson discusses passion for dentistry
"Mrs. Klemmedson, Daniel has eight cavities." The pronouncement, made during a boyhood visit to the dentist, remains ingrained in Dr. Daniel Klemmedson's mind.
"I spent way too much time in the dentist's office," said Dr. Klemmedson. In spite of all the time he spent in the dentist’s chair, it was beside the chair where Dr. Klemmedson saw his future. As he remembers it, he was attracted to the convenience.
"I liked the fact that my dentist in Tucson lived in his office," Dr. Klemmedson said. "His office was attached to his house, and I thought that was pretty cool. "What started out as a career of convenience — either be a dentist or marry a dentist — became a passion, layered with greater complexity than what he had imagined as a teenager.

"What other profession allows for full use of intellectual abilities as well as surgical skills?" he asked. "We are the definition of primary care: Diagnosis, education, prevention and clinical care over a lifetime. The autonomy of practice choice, self-regulation and work-life balance cannot be beat."Dr. Klemmedson's career in organized dentistry will culminate Oct. 19 when he is installed as the 157th president of the American Dental Association at the virtual House of Delegates meeting. Because of the COVID-19 pandemic, the ADA Board of Trustees voted to hold the ADA FDC 2020 meeting and subsequently the House of Delegates virtually this year.
'I didn’t know how to stop'Dr. Klemmedson was born in Missoula, Montana, in 1954. His father's job in forestry and watershed management and his doctoral research at the University of California-Berkley forced the family to move around a bit during Dr. Klemmedson's youth: California, Boise, Idaho, and finally, Tucson, Arizona, where Dr. Klemmedson finished junior high, high school and ultimately obtained a bachelor's degree in biology from the University of Arizona.During a college summer, he served as a counselor for Camp Wildcat, a student-run organization at the University of Arizona that provided underprivileged children the opportunity to go camping in the mountains outside Tucson.
It was there he met another counselor: his wife, Adaline. They ultimately married before he started dental school at the University of Southern California in 1976.
Adaline got a job in the fundraising and development division for one of the vice presidents at USC, and benefited from a program to reduce Dr. Klemmedson's dental school tuition by half. A good portion of the remainder of his tuition was paid by the state of Arizona, which had no dental schools at the time so they collaborated with neighboring states to help residents financially.
As a result, Dr. Klemmedson graduated dental school relatively debt free. Without the debt and the stress that typically comes with it, Dr. Klemmedson had a lot more choices when it came to his next steps. His choice? More school."I did not know how to stop," Dr. Klemmedson said.Dr. Klemmedson completed a three-year oral and maxillofacial surgery residency at the Los Angeles County/USC Medical Center in 1983, obtained his medical degree from the University of Southern California School of Medicine in 1985 and completed a transitional internship in the Tucson Hospitals Medical Education Program in 1986.

You read that right: Dr. Klemmedson is a dentist, oral surgeon and M.D.After obtaining all of his degrees, Adaline ultimately put her foot down."Do you like what you do?" she asked. The answer was yes."Then get a job," she responded.
Dr. Klemmedson met his future partners while providing anesthesia for them during a clinical rotation at Tucson Medical Center. Drs. Theodore Kiersch and Edward Schneider were involved in organized oral surgery and invited him to a meeting at the Western Society of Oral and Maxillofacial Surgeons before he joined their practice."One of my partners became a trustee of the American Association of Oral and Maxillofacial Surgeons," said Dr. Klemmedson.
"I was constantly surrounded by organized dentistry and experienced the benefits first-hand."Dr. Klemmedson eventually became president of the Arizona Dental Association, vice chair of the ADA Council on Dental Benefit Programs, a member of the ADA Board of Trustees and now president-elect.He's switched partners a few times and currently has a practice in Tucson and a satellite one in Sierra Vista, Arizona, less than 10 miles from the Mexican border, where many of his patients come from the Fort Huachuca military base or are veterans from the area.For the past 30 years, Dr. Klemmedson has joined primary care and specialty physicians, audiologists, nutrition specialists, sociologists, dentists, orthodontists and oral and maxillofacial surgeons as a member of the Children's Clinics' cleft palate-craniofacial team.
Dr. Klemmedson coordinates surgical care with plastic surgeons and ear, nose and throat surgeons to address the many specific needs his pediatric patients require from birth to adulthood. His primary area of concentration is with the maxillary cleft closure and bone grafting, orthognathic surgery and dentoalveolar surgery.
During the little free time he does have, Dr. Klemmedson "putters around the yard" with his cacti and succulents; exercises every morning at 4:30 a.m.; is an avid cyclist, having ridden across major portions of Australia; and supports his wife's endeavors."My wife, she's kind of the star of the family to be honest," Dr. Klemmedson said. "She leads and I follow."Adaline ultimately became the program director of the Institute for Marine and Coastal Studies at USC.
In Tucson, she also worked in health care, ultimately retiring as a vice president of the teaching hospital associated with the University of Arizona College of Medicine. After retiring, she became a community volunteer and philanthropist "serving as the chair of more local groups in Tucson than I can name," Dr. Klemmedson said.
(08/18/2020)by Kelly Ganski
More Information: https://www.mybestdentists.com/in-the-news/AmericanDentalAssociation
Views: 3,222
ADA 'respectfully yet strongly disagrees' with WHO guidance recommending delay of dental care
The American Dental Association released a statement Aug. 12 stating it "respectfully yet strongly disagrees" with the World Health Organization's interim guidance recommending that "routine" dental care be delayed in certain situations because of COVID-19."Oral health is integral to overall health.
Dentistry is essential health care," ADA President Chad P. Gehani said. "Dentistry is essential health care because of its role in evaluating, diagnosing, preventing or treating oral diseases, which can affect systemic health."The ADA Board of Trustees adopted an ad interim policy stating dentistry is essential health care during a video call July 27, and the House of Delegates will consider it as a resolution during its virtual meeting in October.
As U.S. COVID-19 cases began to rise in March, the ADA called for dentists to postpone all but urgent and emergency care in order to understand the disease and consider its effect on dental patients, dental professionals and the greater community, Dr. Gehani said.
Both the ADA and Centers for Disease Control and Prevention then issued interim guidance for dental professionals related to COVID-19, calling for the use of the highest level of personal protective equipment available, such as masks, goggles and face shields.
To minimize aerosols, the ADA guidance also recommended dental professionals use rubber dams and high-velocity suction whenever possible and hand scaling instead of ultrasonic scaling when cleaning teeth.
"Millions of patients have safely visited their dentists in the past few months for the full range of dental services," Dr. Gehani said. "With appropriate PPE, dental care should continue to be delivered during global pandemics or other disaster situations."
(08/13/2020)by Mary Beth Versaci
More Information: https://mybestdentists.com/in-the-news/AmericanDentalAssociation
Views: 3,531
When do babies start teething?
Newborns typically have 20 baby teeth concealed below the gumline. Teething is the process of these teeth erupting through the gums.
Teething usually begins about halfway through the first year of life. Different teeth erupt at different rates, with the front teeth tending to emerge first.

During teething, a baby may feel pain and discomfort, and they can show this in various ways.
In this article, we give a general timeline for the eruption of baby teeth. We also describe signs of teething and provide tips on easing any pain and discomfort.
According to the American Dental Association (ADA), baby teeth tend to appear within the first 6–8 months of life.The first teeth to erupt are usually the front teeth at the top or bottom of the mouth. Dentists refer to these teeth as the incisors. The rate and order in which the other teeth appear can differ from one baby to another.The ADA provide the following timeline of the usual ages at which baby teeth emerge:
1. lower central incisors (the bottom front two teeth): 6–10 months
2. upper central incisors (the top front two teeth): 8–12 months

3. upper lateral incisors (at either side of the central incisors): 9–13 months
4. lower lateral incisors (at either side of the central incisors): 10–16 months
5. upper first molars (behind the upper canines): 13–19 months
6. lower first molars (behind the lower canines): 14–18 months
7. upper canines: 16–22 months
8. lower canines: 17–23 months
9. lower second molars: 23–31 months
10. upper second molars: 25–33 months
If there is no sign of any teeth appearing at about 6 or 7 months of age, this is usually no cause for concern, according to the American Academy of Pediatrics.
By the baby’s first birthday, they should see a dentist, whether or not they have teeth yet.The enamel coating on baby teeth is thinner than that on adult teeth, and so it is more prone to cavities. For this reason, routine dental checkups are important for babies.
Signs of teething:
There are several indications that a baby is teething, including:
1. increased irritability
2. increased crying
3. drooling
4. a rash around the mouth, neck, or chest, caused by drooling
5. gnawing or biting on objects
6. cheek rubbing
7. ear pulling
8. a slight elevation in temperature, but not a fever
At about 6 months of age, when teething usually begins, a baby’s immune system is starting to develop, and the antibodies received from the placenta are wearing off. During this time, babies start developing colds and other viral illnesses.
(08/11/2020)by Jenna Fletcher
More Information: https://www.mybestdentists.com/in-the-news/AmericanDentalAssociation
Views: 3,314
Dentistry is an essential service says the ADA Board of Trustees
The American Dental Association Board of Trustees has adopted an ad interim policy stating dentistry is essential health care to help guide advocacy for the dental profession during the COVID-19 pandemic.
The Board established the ad interim policy via a video call July 27, and the House of Delegates will consider it as a resolution during its virtual meeting in October.
"This policy was created to recognize that dentistry is an essential service. Whether it's the current pandemic, a future epidemic or a natural disaster in a particular area, this policy recognizes the need for people to be able to continue to access the full range of dental services," ADA President Chad P. Gehani said (photo).
"Doing so will help people maintain their oral health and contribute to their overall health. Oral health is integral to overall health — staying well often depends on having access to health care, which includes dental treatment.

"From March 16-April 30, the ADA called for dentists to postpone all but urgent and emergency procedures to help mitigate the spread of COVID-19, keep patients out of overburdened hospital emergency departments and conserve personal protective equipment. By the end of May, most state governments had lifted restrictions on dental offices, but as COVID-19 cases continue to rise in many states, the dental community is concerned governors may again limit dental services to urgent and emergency care, which could negatively impact dentists and the oral health of the public, Dr. Gehani said.
The policy states oral health is an integral component of systemic health and dentistry is an essential health care service because of its role in evaluating, diagnosing, preventing and treating oral diseases, which can affect systemic health.
It advises that the ADA use the term "essential dental care" — defined as any care that prevents and eliminates infection and preserves the structure and function of teeth and orofacial hard and soft tissues — in place of "emergency dental care" and "elective dental care" when communicating with legislators, regulators, policymakers and the media about care that should continue to be delivered during pandemics and other disasters.
"Using the term 'elective dental procedures' implies oral health care is optional and diminishes the evidence validating that oral health is an integral component of overall health," Dr. Gehani said.
The policy also states the ADA will urge state agencies and officials to recognize the oral health workforce when designating its essential workforce during public health emergencies. Government agencies such as the Department of Homeland Security and Federal Emergency Management Agency have already acknowledged dentistry as an essential service.
(08/10/2020)by Mary Beth Versaci
More Information: https://www.mybestdentists.com/resources/AmericanDentalAssociation
Views: 3,392My BEST Dentists Journal Headlines

